




Health Information



Plantar Fasciitis Q&A
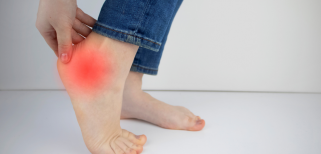
Plantar Fasciitis Q&A (by Michael Roper)
Written by Michael Roper
-
What are the common causes of Plantar Fasciitis?
Plantar fasciitis is often an overuse injury that is primarily due to a repetitive strain causing micro-tears of the plantar fascia. The tears can occur due to trauma or other multifactorial causes:
- An increase in weight bearing activities such as standing, walking or running
- The structure and mechanics of the foot
- The type of shoes you are wearing
- The weight you carry
- Underlying medical conditions
-
What treatment options are available?
Plantar Fasciits’s first line of treatment is usually with conservative measures. Approximately 90% of the cases are treated successfully with conservative care. Conservative care may involve:
- Stretching and Physical Therapy: Massage of the arch and insertion; or stretching and rehab of the plantar fascia, Achilles' tendon, gastrocnemius, and soleus
- Icing and Medication: Ice after activity or oral / topical non-steroidal anti-inflammatory can be used to help alleviate pain
- Rest, Activity Modification and Orthotics/insoles: Relative rest from the offending activity; the level of pain should guide this
- Orthotics/insoles: Shoe inserts, insoles, and night splints may be prescribed in conjunction with the above.
If pain does not respond to conservative care after 3 months treatment, there are still other more invasive options that can be considered:
- Shock Wave Therapy
- Autologous platelet-rich plasma
- Steroid Injections
Conservative treatment is still being conducted while the above treatments are administered
Supposed the condition has become chronic and all other therapies have failed. In that case, surgery may be considered and should be the last option.
-
Are custom-made insoles helpful in this condition?
Using custom insoles for plantar fasciitis can help address some of the causes and relieve the symptoms, allowing the plantar fascia to heal.
-
Will people with flat feet have a higher risk in having Plantar Fasciitis?
Due to the nature of the foot’s mechanic and the loading of the plantar fascia, individuals with low arches/flat feet (pes planus) or those who have high arches (pes cavus) are at risk of developing plantar fasciitis.
-
Should I stop wearing flats or high heels?
Increased High heel wearing is believed to shorten the plantar fascia and the Achilles Tendon, which puts more load onto the plantar fascia compared with normal weight-bearing.
Suppose an individual with poor foot mechanics and acute plantar fasciitis wore an unsupported flat shoe. In that case, it may cause as much pain as wearing high heels.
It is recommended to wear a flat, well-supported shoe with adequate cushioning.
-
How to prevent Plantar Fasciitis?
- When returning to sport, return to with a gradual return to play programme with a good awareness of loading patterns. Have adequate rest after high intensity training days and a general recovery routine.
- Avoid wearing a heel over two inches high. When wearing high heels, take breaks and stretch your feet from your toes to the calves.
- Make sure that your shoes fit; They are not too tight in the front nor too loose that your foot slides around in the shoe.
- A custom orthotic can be placed into the shoes for additional support and padding.
- Reduce prolonged standing.
- Keep your feet and lower limbs fit and healthy.
7. What can I do for immediate relief?
Relative rest from offending activity as guided by the pain level should be prescribed.
Ice after activity, as well as an oral or topical non-steroidal anti-inflammatory can be used to help alleviate pain.
Deep friction massage of the arch and insertion with a tennis ball.
8. What exercises or stretches should I do?
Base of the foot Roll
While seated, grab a tennis ball, rolling pin, frozen water bottle, or other cylindrical object and put it under your foot. Gently roll the object underneath the arch of your foot.
Perform this exercise for 2-3 minutes for each foot. You can repeat up to two times per day.
Towel Stretch
Grab a towel and put it around your foot. While lying down, extend your leg in front of you. Gently pull the towel toward you while keeping your leg as straight as you can. You should feel your calf muscle stretching.
Hold this position for about 30 seconds and repeat 3 times with a break in-between each set. you can repeat this two times per day.
Toe Stretch
In a seated position, push your leg out so that just your heel is on the floor. Bend down and grab your big toe, bending it backwards. While doing this, flex your ankle up that it pulls away from the floor.
Hold this position for about 30 seconds and repeat 3 times with a break in-between each set. Repeat this exercise multiple times per day.
Toe Curls
Put a towel flat under your foot (try to find a smooth surface to do this on) while seated. The goal is flatten your toes and then scrunch them up to pull the towel towards yourself using only your toes.
Perform this exercise by pulling a small hand towel along its’ full length 10 times. You can repeat it one to two times per day.
Calf Stretch
Stand facing a wall with one foot in front of the other. Keeping the back leg straight, lean your weight forward, bending into the front knee. Make sure your back heel stays on the ground and you should feel a stretching in your calf muscle.
Hold this position for about 30 seconds, take a break, and repeat twice. You can repeat this exercise four times a day.
.
9. Will exercises like running make it worse? Should I stop all my activities?
Depending at which stage of the condition, general activities are recommended. The key is that the activities do not overload the fascia, and there is no increased pain during the activity and the pain the following morning is manageable.
Impact exercises like running may make the condition worse depending on:
- The severity of the condition you are in
- The amount of load/capacity you have trained the system to handle.
Returning back to running should be carefully managed and using a load/pain diary would be useful.
References:
- Lemont H, Ammirati KM, Usen N. Plantar fasciitis: a degenerative process (fasciosis) without inflammation. Journal of the American Podiatric Medical Association. 2003 May;93(3):234-7
- Thomas JL, Christensen JC, Kravitz SR, et al. The diagnosis and treatment of heel pain: a clinical practice guideline-revision 2010. J Foot Ankle Surg. 2010;49(3 Suppl):S1–19.



